Breast Augmentation with Silicone Implants – What Should I Consider?
Breast augmentation is one of the most frequently performed aesthetic surgical procedures worldwide. Modern silicone implants allow very precise planning of shape, projection, and symmetry and provide immediately visible and well predictable results.
- Historical background
- Established implant manufacturers
- Implant position
- Surgical access routes
- Surgical procedure and hospital stay
- Downtime and aftercare
- Planning the correct implant size
- Choosing the appropriate implant shape
- Myths, longevity, and implant exchange
- Complications and side effects
- Capsular contracture
- Cost of breast augmentation in 2026
- Surgery abroad – lower cost but increased risk
- Alternative breast augmentation with autologous fat
Historical background
The first successful breast augmentation using silicone implants was performed in 1962. The procedure took place in Houston, Texas. Despite the enormous technical progress since then, all modern implant systems are fundamentally based on this innovation from 1962.
The procedure became truly established only with the development of modern silicone implants, improved surgical techniques, and clearly defined medical standards. Today, breast implants are highly advanced medical devices with tested shells, cohesive silicone gels, and strict quality controls.
Established implant manufacturers
There are several well established breast implant manufacturers worldwide. In Germany, Polytech ® Health & Aesthetics plays a particularly important role, as its implants are developed and manufactured in Germany (“made in Germany”). Polytech ® offers a wide range of implant shapes, projections, and surface technologies.
Other internationally established manufacturers include Mentor®, Motiva ® and Allergan ® depending on market availability.
However, the decisive factor for a good outcome is not the manufacturer alone, but the correct implant selection combined with meticulous surgical planning and precise operative technique.
Implant position
Implant positioning is not a simple black and white decision. Traditionally, implants are placed either above or below the pectoral muscle. In clinical practice, however, a hybrid approach is most commonly used: the so-called dual plane concept, where the implant is positioned partly beneath the muscle and partly beneath the breast gland.
Placement above the muscle can look very natural and is often associated with less early postoperative pain. However, it requires sufficient soft tissue coverage to prevent visible or palpable implant edges. In very slim patients, visible edges or rippling may occur. With increasing age, subcutaneous fat can diminish, potentially making the implant more visible or palpable over time.
Placement beneath the muscle can provide improved soft tissue coverage in patients with little native tissue. The early recovery phase may be slightly more uncomfortable, and in some sports or with strong pectoral muscle activity, implant movement can occur. The appropriate implant position depends not on trends, but on skin thickness, glandular tissue, baseline breast shape, lifestyle, sports activity, and the desired aesthetic result.
The dual plane technique is a well established and widely used method in breast augmentation, as it combines the advantages of both submuscular and subglandular placement. The implant is positioned under the muscle in the upper part and under the breast gland in the lower part. The aim is a natural shape with good soft tissue coverage in the upper pole and a harmonious contour of the lower breast.
This technique is particularly suitable for patients with limited native tissue, mild breast ptosis, or a desire for a natural, non artificial appearance. Partial muscle coverage reduces visible implant edges and rippling, while allowing a soft and natural movement of the lower breast.
Within the dual plane concept, three subtypes are distinguished based on the extent of muscle release and glandular mobility. This classification was introduced by John Tebbetts.
In Dual Plane Type I, the pectoral muscle is released only to a limited extent. The breast gland remains largely in its original position. This variant is suitable for patients with sufficient native tissue, good skin elasticity, and no significant ptosis, aiming for a subtle and natural result with good upper pole coverage.
Dual Plane Type II involves greater muscle release, with partial separation of the lower breast gland from the muscle. This allows the breast to drape more freely over the implant and is particularly useful in cases of mild ptosis or when additional fullness of the lower pole is desired without performing a breast lift.
Dual Plane Type III represents the most extensive variant. The muscle is widely released and the breast gland significantly mobilised, allowing it to glide freely over the implant. This technique is used in cases of more pronounced ptosis or significant skin laxity, when augmentation alone is planned or when a lift is intentionally avoided.
The appropriate dual plane variant depends on multiple factors, including skin elasticity, breast shape, glandular volume, and the desired aesthetic outcome. This is where experience, precise planning, and a refined sense of proportion are essential to achieve a natural and long term stable result.
Surgical access routes
The inframammary fold is the most commonly used approach, as it provides excellent visibility and control.
The periareolar approach (around the areola) may offer discreet scar placement in suitable candidates but requires incision through glandular tissue.
The axillary approach avoids scars on the breast itself but is technically more demanding.
With both the periareolar and axillary approaches, there may be an increased risk of bacterial contamination of the implant pocket, which is discussed as a potential contributing factor to capsular contracture. The use of a the Keller Funnel ® allows insertion of the implant without skin contact and may reduce the risk of capsular contracture.
Surgical procedure and hospital stay
After detailed consultation and surgical planning, preoperative markings are performed with the patient standing. This is important, as breast shape, asymmetries, and the inframammary fold change significantly in the supine position. Surgery is typically performed under general anaesthesia.
After preparation of the implant pocket and insertion of the implants, their position is carefully checked and the wound is closed in layers. Particular attention is paid to tension free placement and precise symmetry. Modern suturing techniques allow for nearly invisible scars.
Following surgery, patients remain for one night in a private clinic. This overnight stay allows for optimal pain control, monitoring of circulation, and early assessment of swelling and wound conditions. Especially during the first postoperative hours, this provides additional safety and a more comfortable start to the recovery process.
The following morning, a postoperative review is performed, the breasts are re examined, and detailed postoperative instructions are discussed before discharge.
Downtime and aftercare
The first few days are typically characterised by tightness, swelling, and a muscle soreness like sensation, particularly when the muscle is involved. Many patients are able to resume normal daily activities after approximately 7 to 14 days, while strenuous physical activity and sports should usually be avoided for several weeks.
Important early postoperative rules include avoiding prolonged arm elevation, not sleeping prone, avoiding sudden movements, and consistently wearing the recommended supportive bra. Depending on the technique and findings, massage, implant mobilisation, or deliberately no massage may be advised. This is always individualised.
Planning the correct implant size
Choosing the implant size is one of the most important steps in breast augmentation and a common cause of dissatisfaction if not carefully planned. This decision is not based solely on volume in cubic centimetres (cc).
Key factors include individual anatomy, chest width, existing glandular tissue, skin elasticity, and the desired aesthetic style. An implant that appears harmonious on one patient may look unnatural or excessive on another.
Therefore, implant sizing systems, precise measurements, and honest counselling play a central role. The goal is always a size that matches the body proportions, remains wearable long term, and still feels appropriate years later. Bigger is not automatically better; balance is what matters.
Choosing the appropriate implant shape
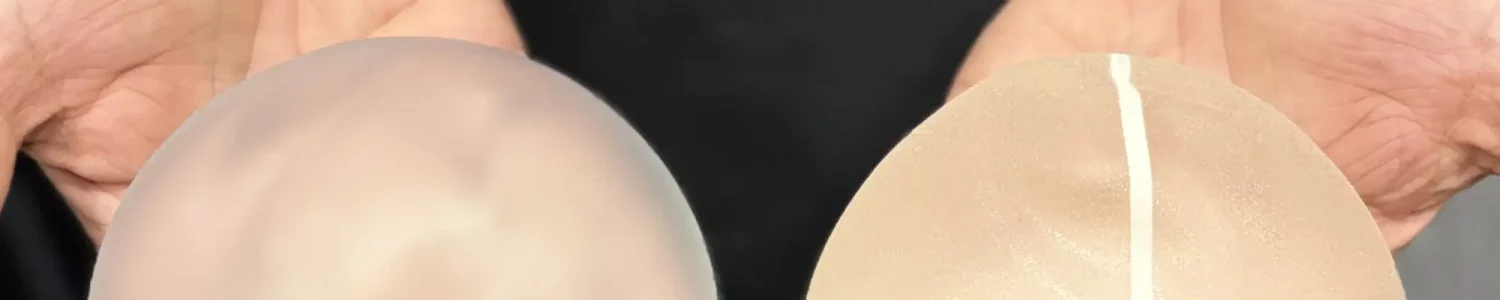
In addition to size, implant shape significantly influences the final appearance. A basic distinction is made between round implants and anatomical (teardrop shaped) implants.
Round implants typically provide more fullness in the upper pole and are suitable for patients seeking a pronounced décolletage. Anatomical implants often appear particularly natural, as they follow the natural contour of the breast, especially in slim patients or those with limited baseline volume.
The appropriate shape depends on the starting breast, skin tension, implant position, and the desired result. There is no universally “correct” implant shape, only the one that is right for the individual patient. Experience and aesthetic judgement are essential here.
Myths, longevity, and implant exchange
Many myths surround breast implants. One of the most common is the assumption that implants must automatically be replaced after ten years. This is not universally true.
Modern silicone implants are durable medical devices. As long as no symptoms, shape changes, or abnormalities occur, there is no fixed time for routine replacement. Regular clinical follow up and, if indicated, imaging studies are important.
Implant exchange may become necessary in cases of capsular contracture, rupture, malposition, or a change in personal preference. Physical changes due to pregnancy, weight fluctuations, or natural ageing can also make adjustment reasonable.
Realistic counselling is essential. Breast implants are neither a lifetime decision without follow up nor a short term product. When correctly selected, properly implanted, and regularly monitored, they can provide stable and attractive results for many years.
Complications and side effects
As with any surgical procedure, risks exist. Short term complications include bleeding, infection, wound healing disturbances, or seroma. Long term complications may include capsular contracture, visible implant edges, rippling, asymmetry, or implant rupture.
An important aspect of modern informed consent includes rare implant associated conditions. BIA-ALCL occurs primarily in association with textured implant surfaces and is considered rare and highly treatable when detected early.
Additionally, BIA-SCC, a very rare squamous cell carcinoma of the capsule, has been reported. Data are currently limited, making thorough patient education and prompt diagnostic evaluation of symptoms essential.
Implants are durable but not “lifetime guaranteed”. Even when they function well for many years, they should be regarded as medical devices requiring ongoing monitoring and appropriate evaluation if symptoms occur.
Capsular contracture
Capsular contracture is a potential late complication following breast augmentation with implants. The body naturally forms a thin connective tissue capsule around every implant, which is a normal and desired process. Capsular contracture refers to an excessive thickening and hardening of this capsule, leading to changes in breast shape or sensation.
According to current data, the lifetime risk of capsular contracture is approximately two to ten percent, depending on implant type, position, surgical technique, and individual tissue response. Modern implants, gentle surgical handling, meticulous haemostasis, and submuscular or dual plane placement can significantly reduce this risk.
Clinically, capsular contracture is classified using the Baker grading system.
Grade I presents with a soft, painless, and normal appearing breast.
Grade II involves slight firmness without visible changes and is usually asymptomatic.
Grades I and II typically do not require treatment.
Grade III is characterised by marked firmness with visible distortion or implant displacement, with or without pain.
Grade IV represents the most severe form, with a hard, painful, and visibly deformed breast, usually requiring surgical correction.
Typical symptoms include increasing firmness, tightness or pain, changes in breast shape, or asymmetry. Capsular contracture may develop months or even years after surgery. Regular follow up and early evaluation of changes are crucial for timely management and preservation of the result.
Cost of breast augmentation in 2026
The question of cost is one of the most frequently asked prior to surgery and understandably so, as it depends on multiple factors and is individually calculated.
In Germany, the price for breast augmentation with silicone implants in 2026 typically ranges from approximately €4,500 to €9,000, depending on the clinic, implant choice, surgical access, anaesthesia, and the inclusion of overnight stay.
Some clinics advertise lower entry prices, while others calculate higher fees that include premium branded implants, hospital stay, and structured aftercare.
Costs should include consultation and planning, implant materials, operating time, anaesthesia and monitoring, clinic stay (for example one night for pain control and observation), postoperative care, and compression garments.
Prices may vary further when additional procedures such as breast lifts or implant exchanges are combined.
Internationally, costs differ significantly. Procedures in some European countries or Turkey are often cheaper than in Germany, while prices in the United Kingdom, Australia, or the United States are typically higher.
Surgery abroad – lower cost but increased risk
Breast augmentation abroad is often offered at significantly lower prices. These differences are usually due to lower staffing and operational costs, shorter hospital stays, and highly standardised processes. Important components such as thorough preoperative assessment, high quality implants, overnight monitoring, or reliable aftercare are often limited or excluded.
A key issue is postoperative follow up. Breast augmentation does not end on the day of surgery. Regular reviews, wound checks, and early detection of complications are essential. When surgery is performed abroad, structured aftercare is often inadequate. If complications occur, they usually have to be treated after returning home, resulting in additional cost and stress.
Early air travel after surgery may increase swelling, impair wound healing, and elevate the risk of thrombosis.
Alternative breast augmentation with autologous fat
As an alternative or supplement, breast lipofilling using the patient’s own fat can be considered. The main advantage is the absence of foreign material and a very natural appearance and feel. Additionally, tissue quality may improve. Limitations include the achievable volume per session and variable graft survival, as part of the fat is naturally resorbed.
If you are interested in this option, detailed information on technique, graft survival rates, aftercare, and BEAULI can be found in the previous blog article on autologous fat transplantation.